Can the CVS Health/Aetna Merger Reduce Emergency Room Use for Minor Problems?
The CEOs of CVS Health and Aetna have said that the companies' planned merger will reduce health care costs for consumers, perhaps through increased use of MinuteClinics. However, two recent studies suggest that greater reliance on retail clinics, at least in their current configuration, isn't likely to lower spending.

This post was researched and written with help from Frontier Group intern Emily Schneider.
CVS Health agreed to buy Aetna, a large health insurance company, for $69 billion late last year. This merger would shake up the health care industry as CVS Health is not only a pharmacy chain, but also a pharmacy benefit manager, a company that negotiates drug prices and manages prescriptions for insurance companies.
The CEOs of the companies have said that the merger will reduce health care costs for consumers. It’s not clear how this will be done, though many news articles have focused on the elimination of the “middleman” in prescription benefits and the possibility that expanded MinuteClinics could divert care from emergency rooms.
CVS currently operates over 1,000 MinuteClinics across the country. These store-based “retail” clinics can treat minor illnesses and injuries, such as strep throat or sprains. Additionally, these clinics offer common vaccinations and perform basic screenings. Many insurance companies cover the cost of care at MinuteClinics, or patients can pay out of pocket.
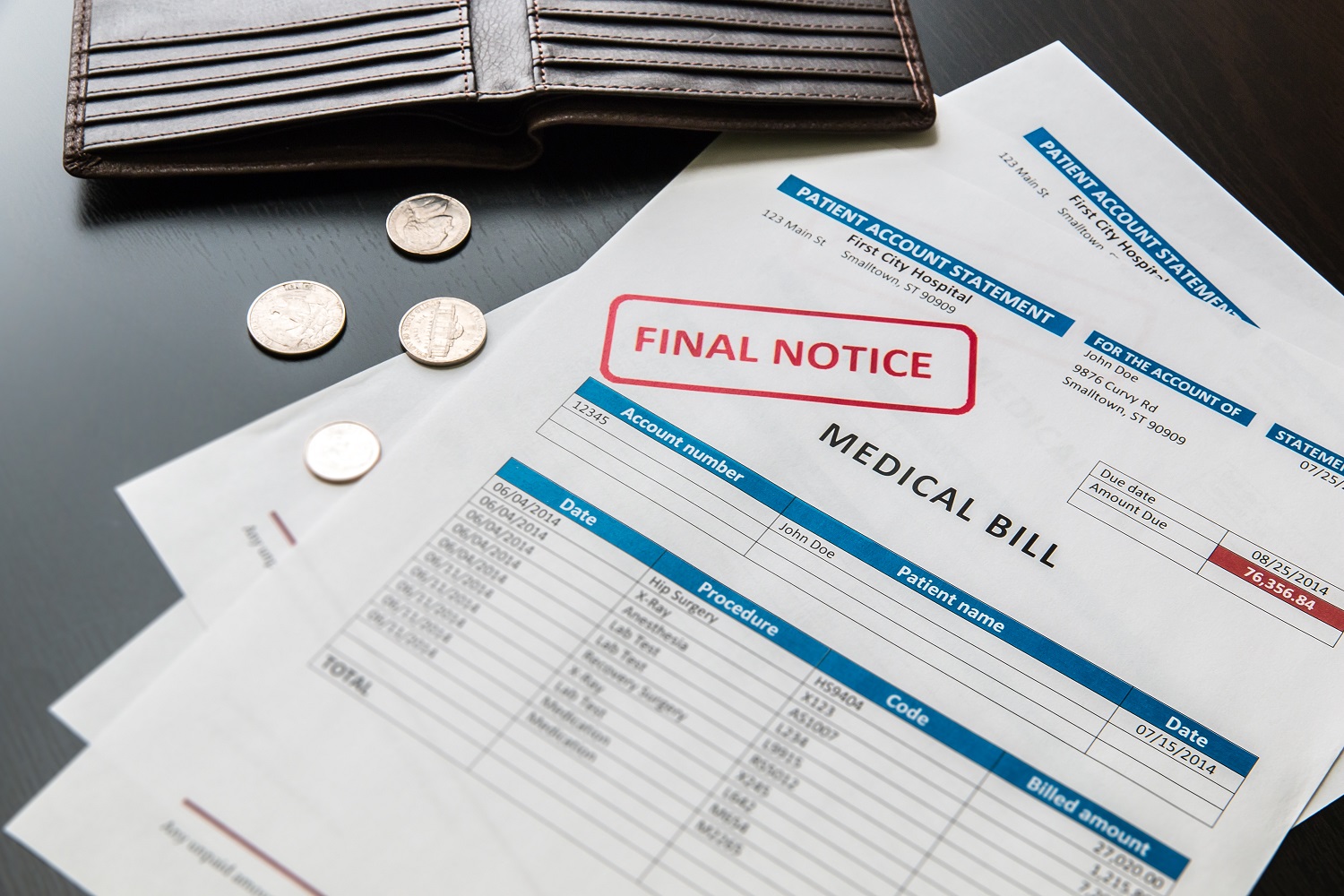
Retail clinics like MinuteClinic are significantly cheaper than traditional health care providers, charging about 70 percent of what urgent care centers and primary care physicians do, and less than one-fifth of an emergency room. For many kinds of care, if patients go to a retail clinic instead of to a traditional provider, they may spend less out of pocket or their insurance company may spend less, potentially passing along savings to consumers through lower premiums or lower copays.
However, two recent studies suggest that patients do not use retail clinics instead of more expensive providers. Rather, they often use retail clinics when they otherwise wouldn’t have sought care at all. This may result in better care and better health, but it doesn’t lower spending.
A 2016 study published in the Annals of Emergency Medicine examined whether the increased availability of retail clinics impacted the number of emergency room visits for minor ailments, such as bronchitis and conjunctivitis (pink eye), that can also be treated at retail clinics. The researchers used data from 2007 through 2012, a period in which retail clinics were becoming more popular. They found that emergency rooms located close to one or more retail clinics saw nearly as many visits for low-level health issues as did emergency rooms with no retail clinics nearby. Retail clinics reduced visits for minor problems by less than one percent. The study concluded that “retail clinics may emerge as an important care location, but to date, they have not been associated with a meaningful reduction in low-acuity ED [emergency department] visits.”
A separate study by researchers at RAND examined the impact of retail clinics on health care spending for more than 13 million patients insured by Aetna from 2010 to 2012. The researchers found that patients visited retail clinics mostly for minor ailments for which they otherwise would not have sought care. Thus, their visits to retail clinics did not replace visits to a traditional provider or an emergency room. Additionally, the use of retail clinics was linked to a small but significant annual increase in health care spending of $14 per person. The researchers concluded that “[t]hese findings do not support the idea that retail clinics decrease health care spending.”
Increased spending is not necessarily a problem. If people decide to get a bad cough checked at a MinuteClinic instead of staying home, that clinic is providing those patients with needed care. And increased access to basic health care is an important goal. But there’s potential downside: the increased availability of retail clinics may decrease the quality of care they receive, by weakening the continuity of care and reducing their visits to providers who offer more comprehensive care. A 2012 RAND study found that patients who visited a retail clinic for a minor problem were subsequently less likely to visit their primary care provider for a similar problem. That’s potentially worse for patient health, because seeing the same provider repeatedly results in better outcomes for patients. (This discussion assumes that MinuteClinics will continue operating as they have in the past. However, they may have less effect on the continuity of care if CVS Health and Aetna fully incorporate MinuteClinics into the new company’s health system, with integrated health records and improved communication between retail clinics and primary care providers.)
The CVS/Aetna merger will likely shake up the health care market, and the integration of an insurance company and a pharmacy benefits manager may deliver efficiency improvements and cost savings. However, while the newly merged company may be able to expand access to basic health care and allow patients to receive care more conveniently, research suggests that in their current configuration MinuteClinics will not reduce emergency room utilization and may increase health care spending rather than reduce it.
Photo credit: Rupert Ganzer via Flickr, CC BY-NC-SA 2.0.
Topics
Authors
Elizabeth Ridlington
Associate Director and Senior Policy Analyst, Frontier Group
Elizabeth Ridlington is associate director and senior policy analyst with Frontier Group. She focuses primarily on global warming, toxics, health care and clean vehicles, and has written dozens of reports on these and other subjects. Elizabeth graduated with honors from Harvard with a degree in government. She joined Frontier Group in 2002. She lives in Northern California with her son.
Find Out More
Developing the antibiotics we need

How useful are hospital price transparency tools?
More and better testing would protect us from chemical threats