Why I Will Continue to Worry about Antibiotic Resistance
As a mother, I have no shortage of things to worry about. There are the mundane concerns, such as: did I remember to pack a snack in my son’s backpack today? has he been exposed to lead dust from the old windows in our house? How do I keep him safe in the car? And then there are the big worries that come with raising a child in 21st century America: how will global warming affect his health, security and the society he will live in as an adult? Will rising health care costs prevent him from getting the care he needs when he is old? And a worry that recently came onto my list: will antibiotics still work in 50 years?
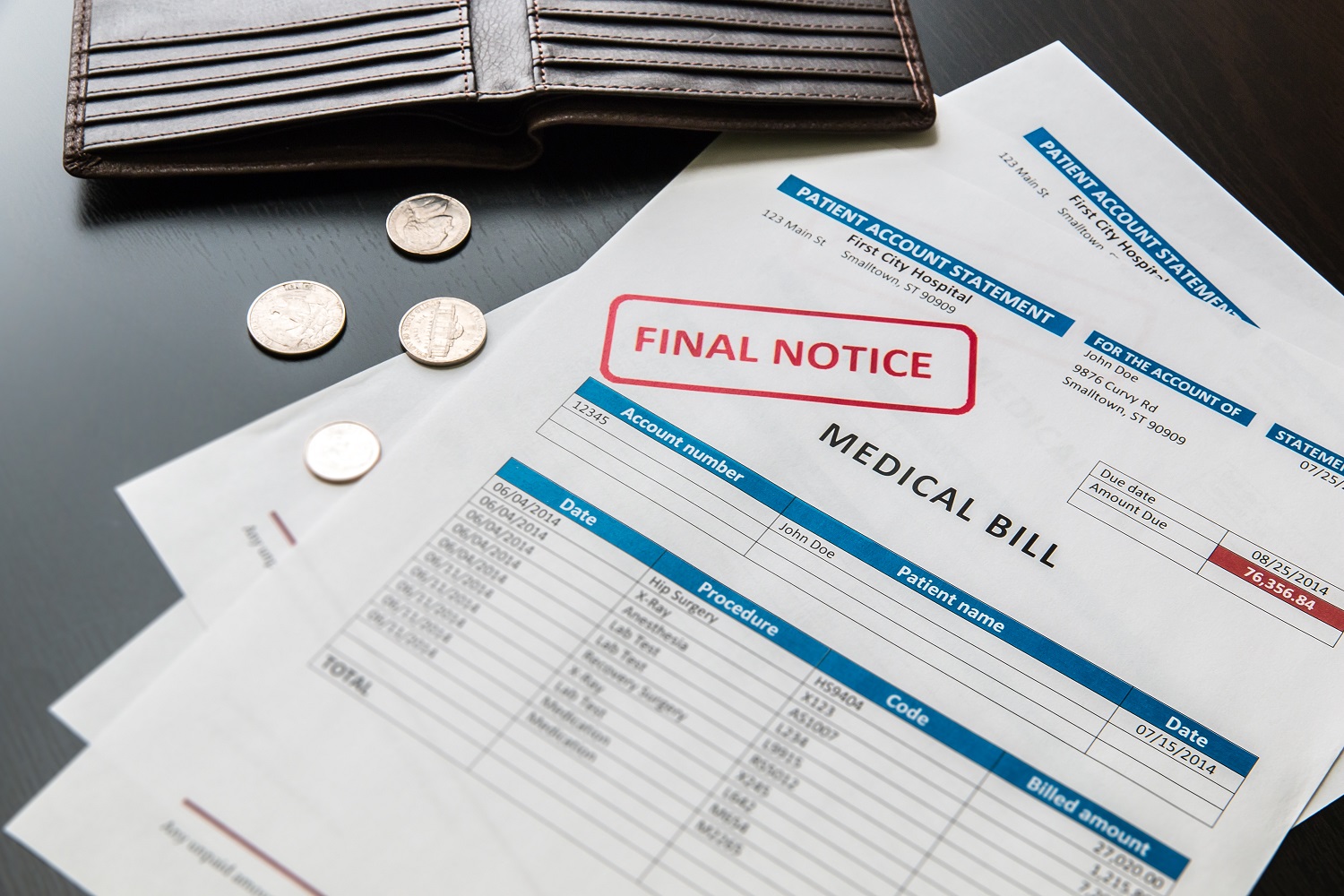
As a mother, I have no shortage of things to worry about. There are the mundane and relatively trivial concerns, such as: did I remember to pack a snack in my son’s backpack today? Does he need bigger shoes? There are the mundane and significant worries: has he been exposed to lead dust from the old windows in our house? How do I keep him safe in the car? Are his toys toxic? And then there are the big worries that come with raising a child in 21st century America: how will global warming affect his health, security and the society he will live in as an adult? Will rising health care costs prevent him from getting the care he needs when he is old? What does rising income inequality mean for social stability, democracy and his economic future? And a worry that recently came onto my list: will antibiotics still work in 50 years?
I can’t worry about all of them or I’d never sleep, so I prioritize what to worry about. What poses the biggest risk to my child today? In the future? What can I do to lessen the risk? The answers for the near-term are pretty easy. For example, car accidents are a leading cause of death for young children, therefore I should take more precautions about car safety than poisoning hazards.
The big, long-term worries are harder to set aside or to do anything about. Working for Frontier Group helps me feel I’m engaged in protecting everybody’s future, but the job includes the occupational hazard of learning about all the problems of the world.
One problem I learned about last year while working on a report about the overuse of antibiotics on factory farms is that antibiotic-resistant bacteria infect more than 2 million people per year in the United States, causing more than 23,000 deaths. Without antibiotics, common diseases like bacterial meningitis or pneumonia could once again be fatal diseases. If bacteria become even more widely resistant to antibiotics—which is the path we are currently on—my son could live in a world where even minor surgery could be a life-threatening procedure because of the risk of uncontrollable infection.
To protect these drugs that are so important to public health, the U.S. needs better policies to limit the formation and spread of antibiotic-resistant bacteria. Key to this is ending the use of antibiotics to make animals grow faster or keep them from getting sick because they are raised in crowded, unhygienic factory farms. Despite the obvious need for this change, it has been an uphill fight. (See what our partners at USPIRG have been doing on this.)
So when I heard of the recent discovery of a new type of antibiotic that bacteria might not become resistant to, I thought I could quit worrying about factory farms that feed antibiotics to animals and in the process create superbugs that lead to deadly infections in people.
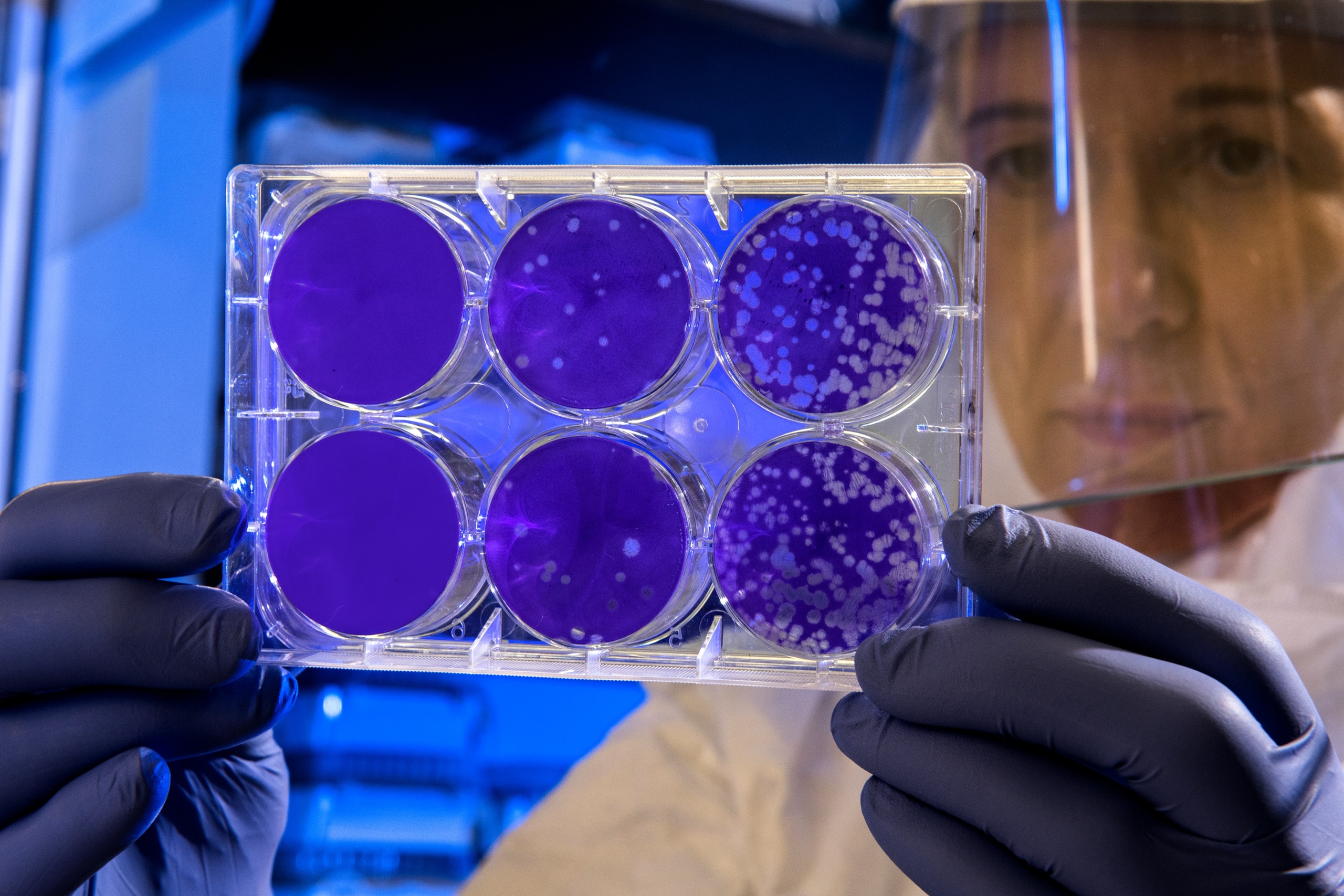
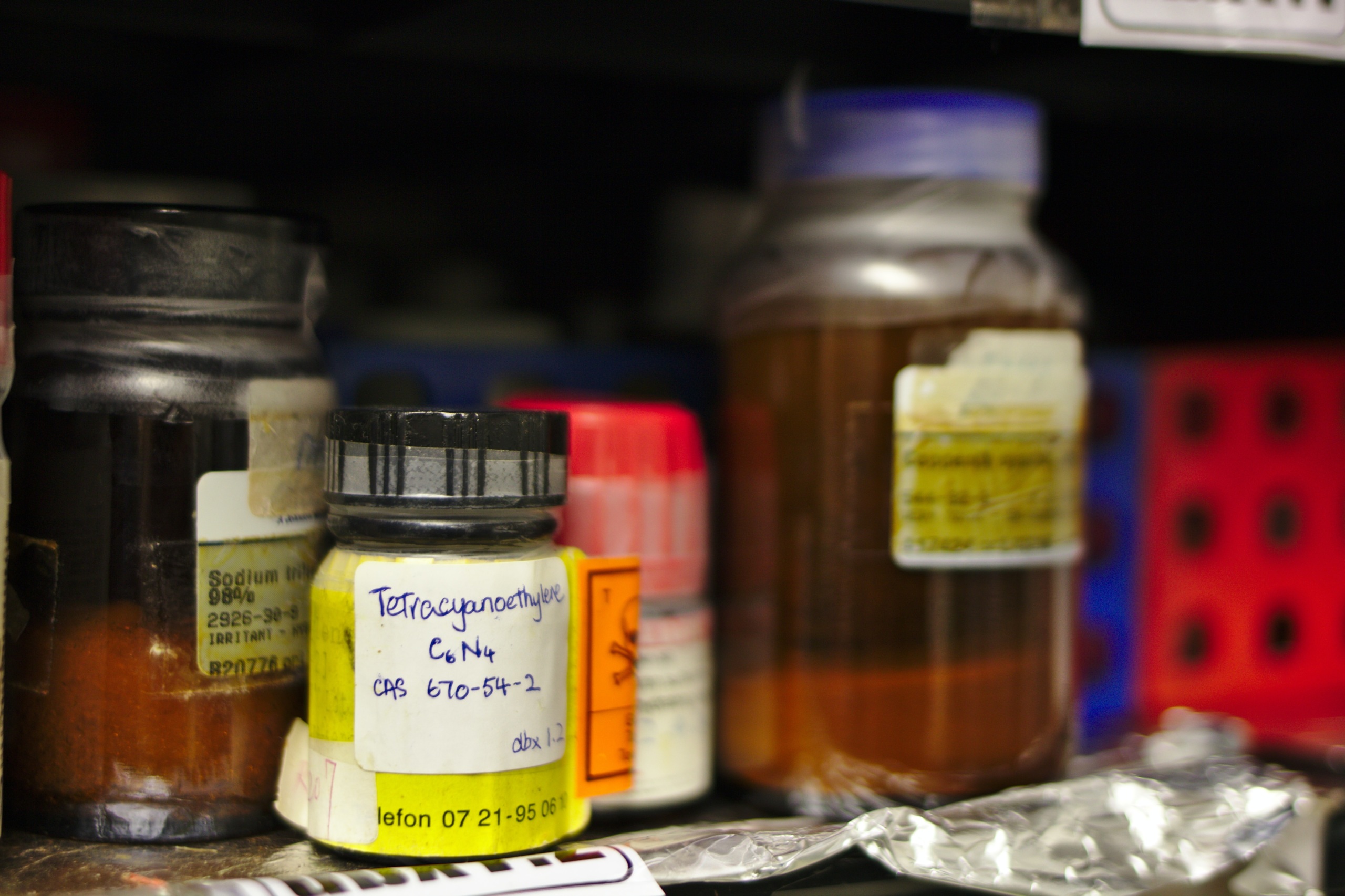
Researchers from several universities and pharmaceutical firms have identified an antibiotic from soil that has demonstrated the ability to wipe out infections in mice—and which bacteria haven’t been able to evade. The new antibiotic, teixobactin, attacks bacteria through a different mechanism than other antibiotics. As a result, bacteria have a much harder time developing resistance. The researchers estimate that bacteria might need three decades to develop resistance to teixobactin, versus just a few years for a typical new antibiotic. The hope is that teixobactin, if it performs as well in humans as in mice, could treat drug-resistant infections caused by bacteria that are impervious to current antibiotics. Adding to the promise behind this drug is the fact that the researchers believe many more antibiotics could be developed from dirt. With effective new antibiotics in the pipeline, we don’t need to worry so much about maintaining the effectiveness of current antibiotics.
Except, after reading a few more articles about teixobactin, I’ve learned more about its limitations. It needs to go through years of trials, and many drugs that have been promising in mice have been toxic or otherwise failed in people. Even if it is successful in people, the drug will have to be injected, which makes it harder to use than many current antibiotics. And, most importantly, at this point teixobactin has no impact on the bacteria that cause pneumonia, gonorrhea, or blood and bladder infections.
I’ll be keeping antibiotic resistance on my list of things to worry about and to fight against. It will stay there until we have better policies to ensure the long-term viability of antibiotics, both those we already use today and new ones we’re just learning about.
Topics
Authors
Elizabeth Ridlington
Associate Director and Senior Policy Analyst, Frontier Group
Elizabeth Ridlington is associate director and senior policy analyst with Frontier Group. She focuses primarily on global warming, toxics, health care and clean vehicles, and has written dozens of reports on these and other subjects. Elizabeth graduated with honors from Harvard with a degree in government. She joined Frontier Group in 2002. She lives in Northern California with her son.
Find Out More
Developing the antibiotics we need

How useful are hospital price transparency tools?
More and better testing would protect us from chemical threats