Forms and Phone Calls: Patients Pay a Price for Health Care’s Administrative Complexity
I recently spent 45 minutes making calls to straighten out a health care billing problem. Multiply my experience by that of millions of Americans, and we collectively must spend millions of hours on the phone and online each year with insurers and providers to obtain insurance coverage, schedule appointments and straighten out incorrect bills. Many of these activities are a direct result of how complicated our system of providing and paying for care is.
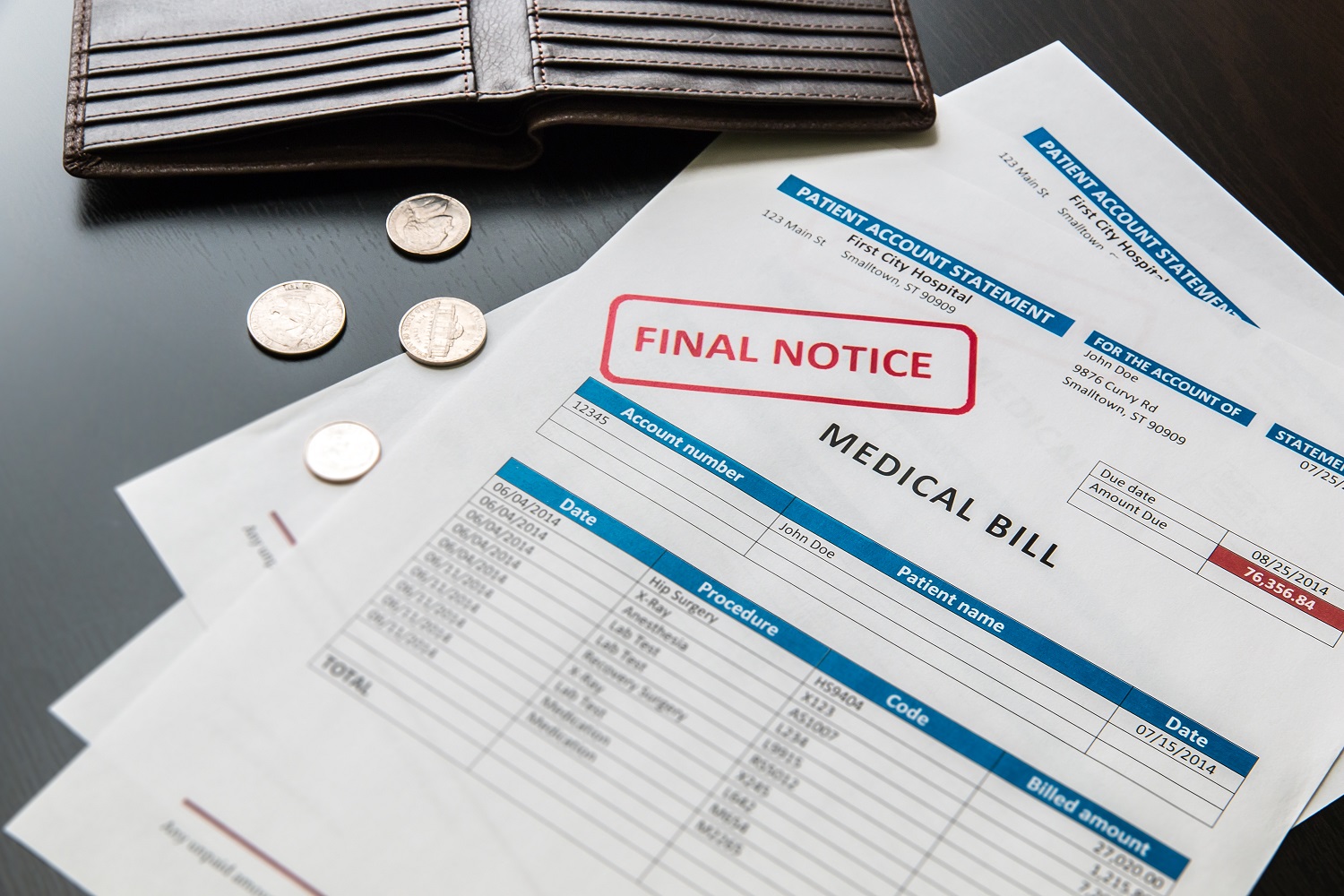
I recently spent 45 minutes calling my health care provider’s billing office, my insurer and the medical group that handles most bills for my insurer, trying to straighten out a billing problem caused when the insurer rejected an expense that should have been approved. Many phone calls later, I figured out that the provider had submitted the bill to the insurer instead of the medical group. Neither the insurer nor the medical group wanted to deal with this problem, though, so it fell to me to call the provider to tell them where to send the bill.
This is the third time this year that I’ve spent a chunk of time untangling insurance and billing issues for my, and my family’s, medical care. Multiply my experience by that of millions of Americans, and we collectively must spend millions of hours on the phone and online each year with insurers and providers to obtain insurance coverage, schedule appointments, straighten out incorrect bills, and clarify insurance details. Many of these activities are a direct result of how complicated our system of providing and paying for care is.
For example, individuals may purchase health insurance through the online marketplaces created by the Affordable Care Act. However, the choices, costs and subsidies are often so complicated that consumers need help figuring out the best option. The Kaiser Family Foundation surveyed experts who help customers navigate the health care marketplace, and found that in 2016 the consultants spent 90 minutes on average with each person who had not previously purchased insurance through the marketplace. For returning customers, the amount of help needed declined – to an hour.
Our fragmented health care system also imposes financial costs on doctors and other providers. Medical providers deal with a multitude of insurers, who each have different pre-approval and reimbursement processes. According to one estimate, the average physician spends more than eight hours a week on administrative activities. Another study concludes that billing and insurance-related activities cost as much as $85,000 per physician per year. In hospitals, a 2014 study estimates that one-quarter of total spending is for administrative expenses, equal to 1.4 percent of the nation’s total economic output.
In addition to raising the financial cost of health care – which is paid for by patients and taxpayers –administrative complexity imposes additional costs on patients. We pay for it through lost time at work (which, for hourly workers, means less income) or reduced leisure time. For example, each time I spend 45 minutes calling my insurer and various billing offices, I lose a portion of my workday and have to work that evening instead of talking to my son or going for a walk.
Reducing patient time spent dealing with insurers and providers on billing and scheduling will require simplifying our very complex and fragmented health care system. For example, insurers could use more “bundled” payments, in which the insurer pays a lump sum for a package of services related to a particular medical problem, instead of paying a la carte for each provider and facility involved. Based on the statements my family receives, I suspect that if my insurer used more bundled payments I might need to review – and correct – fewer billing statements. Another solution might be better integration within provider groups, so that a single organization employs my doctor, runs the lab that draws my blood, and operates the pharmacy where I fill prescriptions. Some health care providers already offer this level of integration, demonstrating its feasibility. Not only would my medical care be better integrated, but a single billing office could handle all invoices to the insurer.
Changes such as these might simplify billing processes within our medical system, thereby reducing the time burden that our health care system imposes on patients and improving their overall experience. In addition, more streamlined billing and insurance may reduce administrative time for medical providers, helping to bring down total health care costs for the nation.
Photo credit: UrbanBohemian via Flickr CC BY-NC-ND 2.0
Topics
Authors
Elizabeth Ridlington
Associate Director and Senior Policy Analyst, Frontier Group
Elizabeth Ridlington is associate director and senior policy analyst with Frontier Group. She focuses primarily on global warming, toxics, health care and clean vehicles, and has written dozens of reports on these and other subjects. Elizabeth graduated with honors from Harvard with a degree in government. She joined Frontier Group in 2002. She lives in Northern California with her son.
Find Out More
Developing the antibiotics we need

How useful are hospital price transparency tools?
More and better testing would protect us from chemical threats